Building a Model for Healthcare in Trenton, Patient by Patient: Health Team Focuses on 45 Frequent Emergency Room Users, Aims to Improve Treatment at Reduced Cost
A project under way in Trenton that aims to improve the healthcare of 45 local residents could pave the way for broader improvements in the area’s healthcare system.
The initiative will focus on 45 people who are among those who use area hospitals’ emergency departments most frequently, including some who made more than 200 emergency visits in the past year.
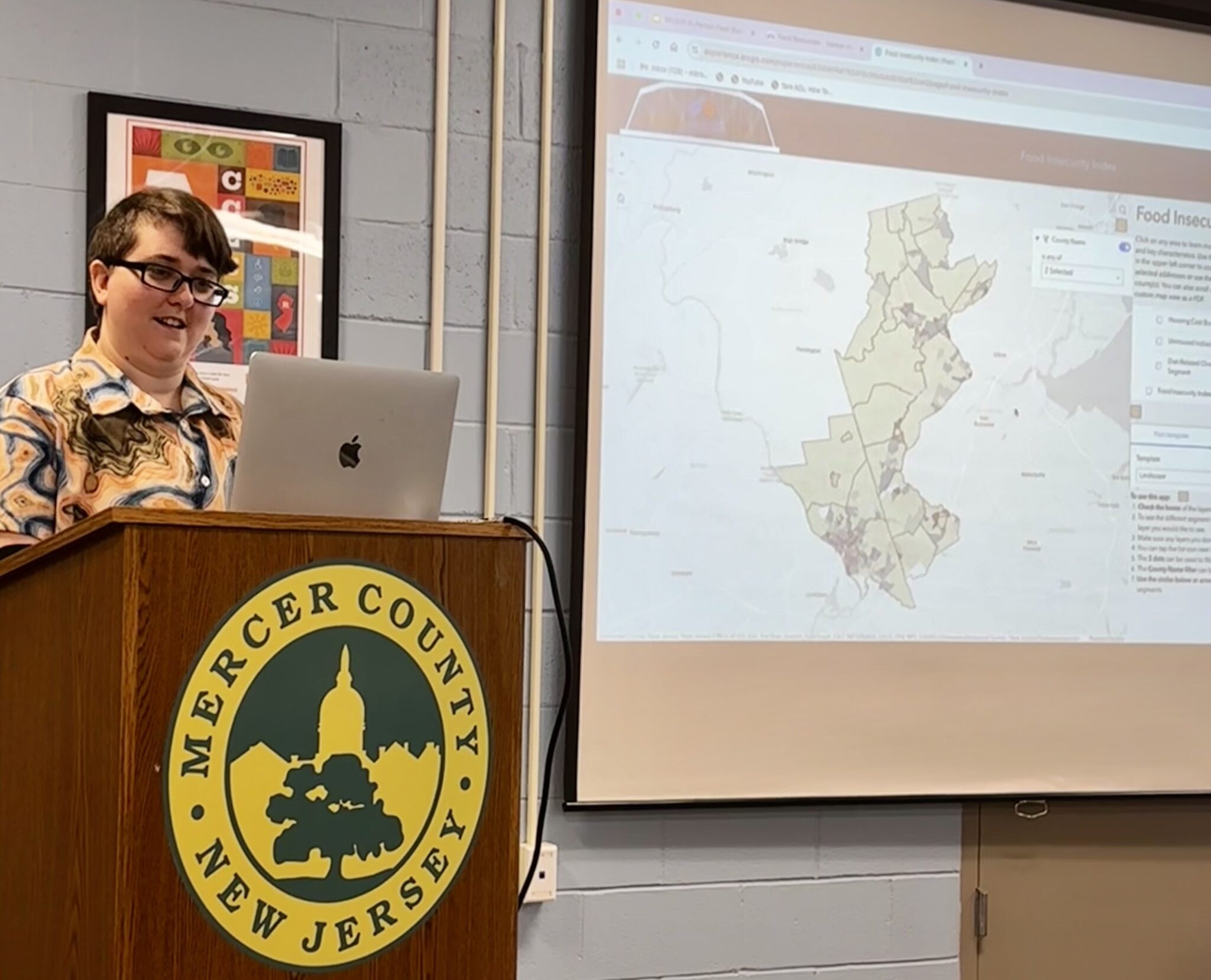
The project is being undertaken by the Trenton Health Team, a partnership between Capital Health Regional Medical Center; St. Francis Medical Center; the Trenton municipal health department; and the Henry J. Austin Health Center, the city’s federally qualified health center.
The four groups are setting up a health information exchange that will allow them to share patient information with the others. They also plan to establish an accountable care organization (ACO), in which Medicaid would pay providers based on patient outcomes and their record of keeping costs down rather than for each service they provide.
The project tracking the care of the 45 people is being funded as part of a $1.5 million grant from the Nicholson Foundation that is intended to help the Trenton Health Team prepare to become an ACO.
A clinical-care coordination team will focus on the frequent emergency patients. St. Francis and Capital Health began referring patients to the team in May and they have enrolled the first 11 people in the program.
“Each case is a lesson for us in how we can better meet the needs of our community,” said Gregory Paulson, deputy director of the THT.
The community health workers on the care coordination team are working with the residents to understand the reasons for the frequent hospital visits and to make sure they are receiving the primary care and social services needed to reduce their hospital visits.
For instance, community health worker LaTanya Bethea said she is working with a program participant whose wife recently died. Team members believe he started visiting the emergency room when he experienced a combination of minor health problems and did not know how to otherwise deal with his situation.
Bethea said she arranged for the man to have prepared meals delivered to his home and to have a visits from volunteers to provide companionship.
THT executives said the care coordination team members’ experience in providing services in the community puts them in a good position to find help for program participants.
“That was a very conscious decision on our part,” said Dr. Ruth Perry, executive director of THT. She said that having team members who understand the community will help in getting residents to participate.
For instance, Bethea previously worked as an detention officer for the Mercer County Detention Center for prisoners who are confined to in-home detentions, while fellow care-team member Kerron Smith previously served as an assistant manager at a group home in Ewing.
THT members believe that taking steps like asking what residents’ needs are and then matching them with primary-care and social-service providers will go a long way toward reducing emergency department overuse.
A community health needs assessment conducted by the hospitals determined that substance abuse and mental health issues, as well as sickle-cell anemia, were among the top reasons for the frequent emergency visits. Each of these issues has cropped up among the first 11 participants in the project.
Dr. Robert J. Remstein, Capital Health’s vice president for accountable care, said the project is part of a shift in thinking about what causes heavy emergency department use. Instead of emphasizing why patients don’t comply with instructions from providers about how to take care of themselves, the THT is focusing on understanding what impediments patients have toward accessing care and understanding the healthcare system.
Perry likened the program to “not only giving a person a fish but also to teach them how to fish.”
She hopes that the lessons the team learns from the project focusing on high emergency-departments users can be applied across the state and potentially across the country, due to the level of cooperation that’s unique to Trenton but may expand elsewhere as health information exchanges grow.
Bethea and Smith have already found that it is difficult to track down some homeless participants to make sure they make appointments with primary-care providers. This has required the care team to be in close contact with the Trenton Area Soup Kitchen and the Rescue Mission of Trenton, a shelter that serves the city’s homeless.
“That’s just really been a difficult issue for us” in the program’s early weeks, Bethea said.
If the 45 participants’ health improves and emergency visits decrease, they will “graduate” from the program and the care team will enroll new participants.
While the program funding is set to expire in February, the Trenton Health Team has been applying for grants to continue it beyond then. In addition, the team is hoping for funding through the potential ACO.
“We really want our care plans to be based on each individual’s needs,” Paulson said. “We view high ER utilization as an indicator that there are other needs and other problems that are not being met – that they’re asking for help in the only way that’s apparent to them.”
The THT is hoping that the project reinforces positive early assessments it’s received from health policy experts in the state.
Joel Cantor, director of the Rutgers Center for State Health Policy, said the team appears “to be making great progress in pulling together a community-wide collaborative. They have all the major players at the table. They’re very well positioned to become certified as a Medicaid accountable care organization.”
Cantor said the Trenton group has been able to learn from providers in Camden and elsewhere.
“They had the advantage of learning from years of experience in Camden in trying to find their way. That means they can get everything up much faster, because they’re not inventing everything from scratch.”
Cantor praised Capital Health and St. Francis with choosing to work together to meet the goals of the 2010 Affordable Care Act.
While all hospitals have to conduct community health needs assessments as part of the ACA, it’s not common for hospitals to work together, Cantor noted.
“That’s a very strong approach to engaging the community,” he said. “It’s very collaborative, instead of each institution going about it on their own, so I think that’s a strength.”
About the Trenton Health Team
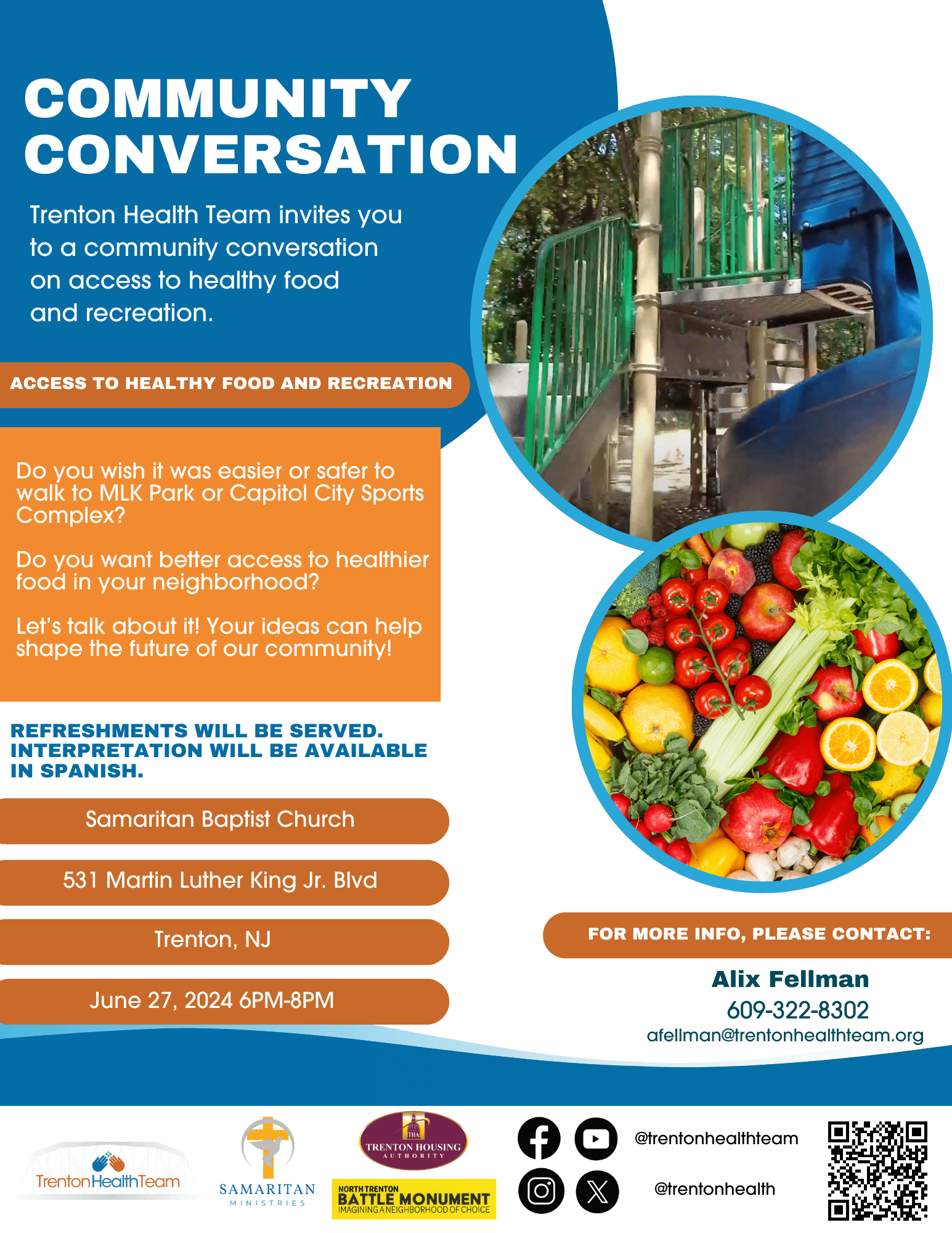
Trenton Health Team (THT) is an alliance of the city’s major providers of healthcare services including Capital Health, St. Francis Medical Center, Henry J. Austin Health Center and the city’s Health Department. In collaboration with residents and the city’s active social services network, THT is developing an integrated healthcare delivery system to transform the city’s fragmented primary care system and restore health to the city. THT aims to make Trenton the healthiest city in the state. Support for the Trenton Health Team was provided in part by a grant from The Nicholson Foundation. For more information, visit www.trentonhealthteam.org.