Robert Wood Johnson Foundation announces new ‘culture of health’ initiative with N.J. leaders
PLAINSBORO – America lags behind other developed countries in life expectancy, teenage pregnancy and childhood obesity rates, John Lumpkin of the Robert Wood Johnson Foundation said Friday.

From left to right: John Lumpkin, senior vice president and director of Targeted Teams at RWJ, Heather Howard, director of the State Health Reform Assistance Network, Ruth Perry, executive director of Trenton Health Team, Annette Catino, president and CEO of QualCare Alliance Networks, and state Department of Health Commissioner Mary O’Dowd. (Nicole Mulvaney/The Times of Trenton)
That’s why the foundation is stepping in to modify the nation’s “culture of health” and work with health care professionals to help Americans lead healthier lifestyles in a variety of ways.
“The only measure we stand up to other countries to and far exceed is the cost of care. And that wouldn’t be so bad if it wasn’t for the fact that we have poor health outcomes,” said Lumpkin, senior vice president and director of Targeted Teams at RWJ. “When you look at it, it’s really some of the choices that we have in our society and the way we live our lives here. Essentially we have a culture that leads to our population being unhealthy.”
Representatives of the foundation held a two-part panel Friday morning made up of local and state health leaders at its headquarters in Plainsboro to debut an initiative to urge policymakers to invest in programs that link health care in hospitals with personal well-being outside of those facilities.
“We have for too long thought about what happens in clinical care and what happens in public health or the community as separate. In fact, you have to build the bridges between those so they both work more closely together and see how one can support the other,” said James Marks, senior vice president and director of Program Portfolios with RWJ.
The forum, moderated by Dan Gorenstein of National Public Radio’s Marketplace, came days before its formal launch Tuesday at the Aspens Ideas Festival in Colorado.
Officials gave New Jersey leaders a sneak peek Friday as Gorenstein posed questions to panelists, which included state Department of Health Commissioner Mary O’Dowd, Department of Agriculture Secretary Douglas Fisher and others including Lee McDonald, director of guidance in the West Windsor-Plainsboro school district, and Ruth Perry, executive director of the Trenton Health Team.
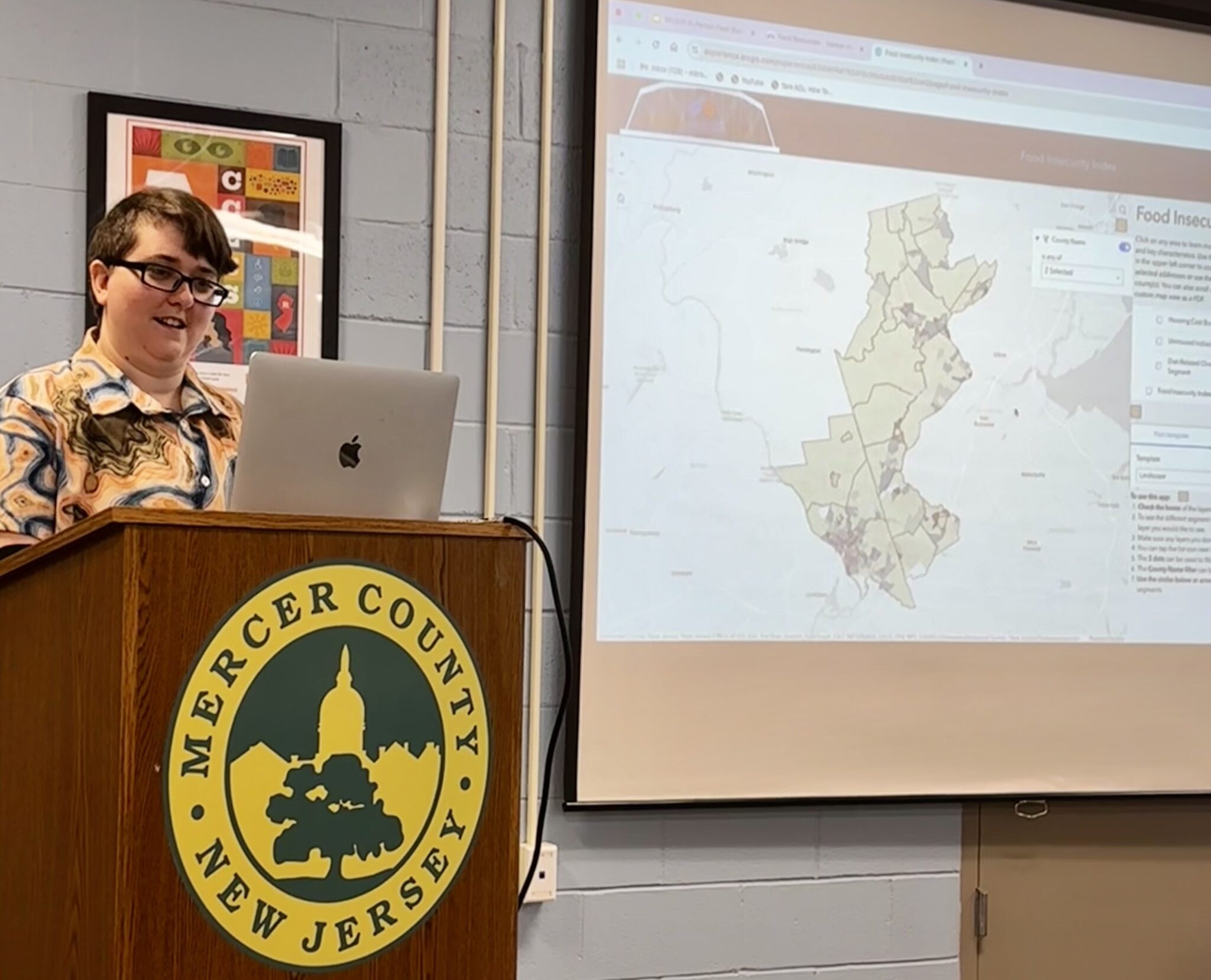
RWJ ranks Mercer eighth and Burlington seventh among the 21 New Jersey counties in terms of health factors, including graduation rates, unemployment, violent crime and air pollution. Programs are starting in which physicians and other health care providers are working with patients to address food insecurity, unstable housing and other social challenges, Marks said.
O’Dowd has been pushing for state hospitals to embrace programs that increase the rate of breastfeeding for newborn babies. She cited statistics yesterday from The Centers for Disease Control and Prevention that show babies who breastfeed exclusively for nine months have a 30 percent reduced risk of childhood obesity.
Four hospitals in New Jersey, including Capital Health Medical Center in Hopewell, are designated “baby friendly,” where staff are trained about breastfeeding and the outcome it has for both a mother and child. Others are on the way to earning that same designation, including University Medical Center of Princeton at Plainsboro.
“It takes time and persistence, but it really raises the standard of how all mothers are going to be supported if they choose breastfeeding,” O’Dowd said.
Following infancy, agriculture officials work with schools statewide to encourage students to make nutritious food choices early on in their development, Fisher said.
“We talk about school gardens, and it’s very much at the forefront these days to get school gardens where children can learn how to nurture and grow food, bring that into the classroom and learn how to prepare foods,” Fisher said. “It has to be tasty, nutritious, presented well, and so we go into the schools with our food service people and the food service companies and try to develop new recipes.”
One of the challenges for RWJ is its restrictions as a private institution; officials cannot engage in lobbying or any political processes, Lumpkin said. But it grants $400 million annually to projects and initiatives that support its mission of improving health across the country, he said.
“We don’t have the resources to affect every community, but we do believe that policy analyses and research and the demonstration that we can actually do better makes a difference,” Lumpkin said.
Government has “good levers, and we need to know how to pull them and push them and hopefully use them in concert” so officials from different departments – health, education and transportation – can work together toward a common goal, said Heather Howard, director of the State Health Reform Assistance Network.
“It’s hard when everyone’s got a tight budget and you’re proposing a new initiative that you think is upon someone else, and they’re worried about their budget and what that means for them,” said Howard, a Princeton councilwoman who serves as council’s liaison to the town’s Board of Health and Human Services Commission. “When you’re dealing with the state, you’re dealing with a one-year budget cycle, so all of us in this room are concerned with return on investment in health in communities, but you can’t always see that in one budget cycle.”
Alonzo Plough, RWJ’s chief science officer, emphasized the importance of ensuring everyone across the nation, regardless of socioeconomic status or ethnic background, has access to high-quality health care, foods and places to be physically active.
“Sometimes a ZIP code is a negative determinate to your health. How do you bring more equity to that? Better housing, safer neighborhoods, walkability, air quality, and so we are going to be doing a lot of work in those areas,” Plough said.
He is working on ways to measure how the “culture of change” manifests itself in communities and on the Web, including tracking how people search for prevention and treatment terms on the internet, he said.
But the issue is particularly complex in cities like Trenton with significant homeless populations, Perry said.
“Many individuals who are homeless and have substance abuse problems, they come to the emergency room because they know it’s warm, they will be fed – this is all the right thing to do, but its not necessarily what the emergency room was designed to do, so the social determinants of health are huge in our community,” Perry said.
About the Trenton Health Team
Trenton Health Team (THT) is an alliance of the city’s major providers of healthcare services including Capital Health, St. Francis Medical Center, Henry J. Austin Health Center and the city’s Health Department. In collaboration with residents and the city’s active social services network, THT is developing an integrated healthcare delivery system to transform the city’s fragmented primary care system and restore health to the city. THT aims to make Trenton the healthiest city in the state. Support for the Trenton Health Team was provided in part by a grant from The Nicholson Foundation. For more information, visit www.trentonhealthteam.org.