Accessing Healthcare, Even if it Starts in the Emergency Room, Should be Applauded
By: Ruth E. Perry, MD – Special To Newjerseynewsroom
I am following the national dialogue about a landmark study called the Oregon Health Insurance Experiment that found that expanding health insurance to low-income households did not decrease use of emergency departments, as had been predicted.It is ironic to read reports that healthcare reform is having the opposite of its intended consequences.All this flurry of fear and angst reminds me of a revival that I attended in October, where the leader asked us to turn to our neighbor and say, “Don’t trip! It’s going to be alright!” I think that this instruction is relevant in our discussion of the Oregon experience.
It is not surprising that newly insured people would begin to avail themselves of medical services and utilize the emergency department to access the healthcare system. Many individuals who were formerly uninsured lack a primary care physician with whom they have established a relationship. Therefore, it is logical that they would go through the easiest route to access care – the ER.
In Trenton, we recently concluded a Community Health Needs Assessment. As part of this process, we conducted over 300 one-on-one interviews and over 30 community forums, and we learned that emergency department utilization is driven by many factors such as poor public transportation, unreliable private transportation, poor health literacy, expensive outpatient practice co-pays, and inconvenient physician hours. It is easier to call an ambulance and receive transportation to the emergency department, which is open 24/7 and cannot turn anyone away.
A longer-term study in Massachusetts, which expanded coverage for its residents in 2006, points to reductions in use over time, finding an 8 percent decline in ER use over several years. It is vitally important to note that in earlier analyses of the Oregon experiment it was noted that, “gaining coverage reduced the incidence of depression and increased feelings of financial stability.” I believe other states will have similar experiences.
Clearly, obtaining insurance coverage is only the first step in turning around the upward spiral of healthcare costs. Improving health outcomes, improving patient experience and reducing healthcare costs require a transformation of healthcare delivery that integrates behavioral health and social services more effectively.
With generous funding from The Nicholson Foundation, Trenton has formed a Community-wide Clinical Care Coordination Team (C4T), composed of physicians, case managers, nurses, and social workers, community behavioral health and social service agencies, from across the community. The C4T focuses on data analysis to identify the highest utilizers and their issues. This collaborative work generated a 45 percent reduction in inappropriate use of the emergency department. When 5 homeless patients received permanent housing, ER utilization dropped by 72 percent and inpatient utilization and charges dropped by 100 percent compared to the previous year.
These early successes enabled us to form a dedicated Care Management Team, which consists of a nurse case manager, a social worker and two community health workers. They are working with a group of 50 patients who have been identified because of their frequent and often inappropriate use of the ER. Many have serious medical conditions that are complicated by social and behavioral issues, including addictions and homelessness. By providing patients with close case management plus social service and behavioral health support, we have experienced reductions in utilization and hospital charges.
I applaud the state of Oregon for their efforts in expanding insurance coverage for their residents and sharing their results with the nation. We should also applaud the newly insured for accessing care. Accessing care is the first step toward earlier detection of chronic illnesses. Earlier detection and treatment will reduce the likelihood of complications, morbidity and mortality, which will reduce costs and improve the quality of life for people over time. As in Massachusetts, inappropriate ER utilization will decrease, especially with close case management and addressing the social determinants of health across the community. So remember, “Don’t trip! It’s going to be alright!”
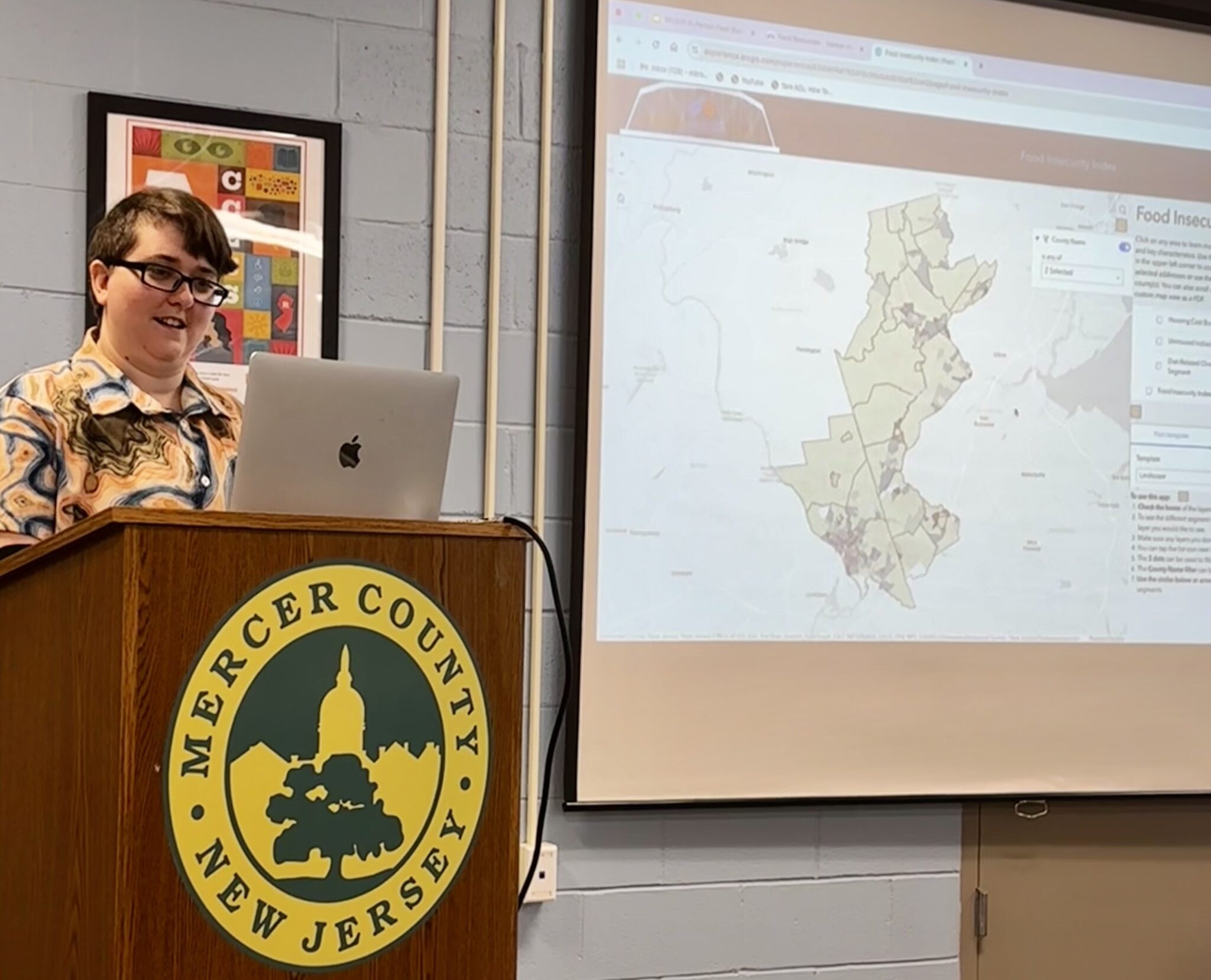
About the Trenton Health Team
Trenton Health Team (THT) is an alliance of the city’s major providers of healthcare services including Capital Health, St. Francis Medical Center, Henry J. Austin Health Center and the city’s Health Department. In collaboration with residents and the city’s active social services network, THT is developing an integrated healthcare delivery system to transform the city’s fragmented primary care system and restore health to the city. THT aims to make Trenton the healthiest city in the state. Support for the Trenton Health Team was provided in part by a grant from The Nicholson Foundation. For more information, visit www.trentonhealthteam.org.
###